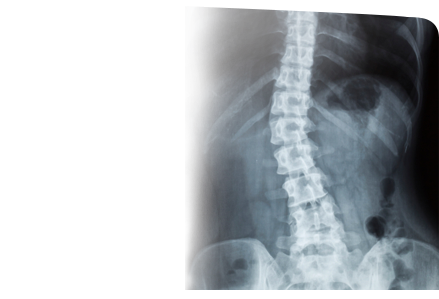
Adult scoliosis is the abnormal curvature of spine giving the spine an “S” or “C” shape in a skeletally mature person. Larger curves cause discomfort while the smaller curves do not cause any problems. In most cases, the exact cause remains unknown. However adult scoliosis can develop as a result of:
- Untreated childhood scoliosis
- Inherent, age-related changes occurring in the body
- Certain diseases affecting the spine
Symptoms of adult scoliosis may include the following:
Uneven shoulder- one shoulder is more prominent and in raised position than the other
Back pain
Head is not in centered position
Abnormal curve of the spine
Breathing problems
Lethargy
Children with scoliosis have some typical physical signs, which include:
- A bulge or hump on one side of the back which appears when bending forward
- Curvature of the spine laterally
- Uneven shoulders and hips
Pain is the predominant symptom in patients suffering from degenerative scoliosis. A compression of the spinal nerve root can result in lower limb weakness along with numbness or tingling sensation. This may hamper coordination and balance with a difficulty in movement, standing or sitting. Occasionally, compression of the lower spinal nerves can also lead to difficulty in urination and defecation. This requires immediate medical care.
Degenerative scoliosis can lead to physical deformities such as humpback, prominence of the rib, altered gait, tilting of the trunk to one side and spinal instability and rigidity.
Diagnosis
Spine surgeons are well experienced in managing back problems. In case of any disorder affecting the spine, contact a specialist immediately as the right diagnosis is crucial for devising an effective treatment plan.
A diagnosis of adult degenerative scoliosis involves:
A detailed medical and family history of the patient
- Neurological examination
- Testing of reflexes to evaluate muscle weakness, sensitivity, and other signs of neurological injury
- Physical examination to evaluate movements at the spine and leg length measurements
Diagnostic imaging techniques such as X-rays, CT scan, MRI scans and myelography may also be used to improve the accuracy of diagnosis.
Treatment
In some patients simple life style modifications such as improved nutrition, smoking cessation and regular exercise may be sufficient for the management of scoliosis. A few patients may respond to non-surgical methods such as analgesics and anti-inflammatory medications, braces, spinal injections, and physical therapy.
Surgery is recommended for patients who fail to respond to non-surgical treatment or the curvature progresses and becomes greater than 45-degrees, or is a cause of cardiopulmonary complications.
Surgery is an option for individuals with severe scoliosis to stop the curve from getting worse. The surgery repairs the abnormal curvature of the spine. There are different surgical approaches to repair the deformity, and the choice of the approach to the spine is based on the type of scoliosis, location of the curvature of the spine, ease of approach to the area of the curve and the preference of the surgeon.
- Anterior approach – It is the procedure in which the surgeon will approach the spinal column from the front of the spine rather than through the back. The incision is made on the patient’s side, over the chest wall or lower down along the abdomen, depending on the part of the spine that requires correction. The lung is deflated and a rib is removed in order to reach the spine. After the exposure of the spinal column, the disc material between the vertebra involved in the curve is removed. Screws are placed at each vertebral level involved in the curve, and these screws are attached to a single or double rod at each level. After instrumentation a fusion is performed, the bony surface between the vertebral bodies is roughened and bone graft is placed. A combination of compression along the rod, and rotation of the rod will correct the spine deformity. The incision is closed and dressed.
- Posterior approach- It is the most traditional approach and the approach is made through the patient’s back while the patient lies on his or her stomach. The incision is made down the middle of the back. Hooks are attached to the back of the spine on the lamina, and screws are placed in the middle of the spine. After the placement of hooks and screws, a rod that is bent and contoured into a more normal alignment for the spine is attached and the correction is performed. After the final tightening, the incision is closed and dressed.
- Anterior and posterior approach – This approach is used in cases where the curve is stiff and severe. The first approach to spinal column is made from the front. The incision is made on the patient’s side, over the chest wall or lower down along the abdomen. Disc material between the vertebrae is removed. This procedure requires removal of a rib, which is later used for bone grafting.
- After the anterior procedure, the wound is closed and the patient is positioned for the posterior approach. The incision is made down the middle of the back. Hooks are attached to the back of the spine on the lamina, and screws are placed in the middle of the spine. After the placement of hooks and screws, a rod that is bent and contoured into a more normal alignment for the spine is attached and the correction is performed. After the final tightening, the incision is closed and dressed.
Possible complications after scoliosis repair surgery may include:
- Nerve damage causing muscle weakness
- Respiratory or lung problems causing difficulty in breathing
- Spine Infection
- Failure of the bone to join together
- Blood loss requiring transfusion
- Blockage of the intestine may occur
- Gallstones may occur
- Movement of the metal hooks placed in the spine
- Pseudarthrosis, a painful condition occurring as a result of non-healing of the bone effusion, and a false joint grows at the site
- Blood clot formation in the legs: is rare but dangerous if they dislodge and travel up to the lungs
- Pain at the bone graft site
Physical therapy is advised after surgery to help the spine grow normally. Physiotherapists evaluate the posture, muscle strength, and flexibility and then design exercise program suitable for patient that helps to control pain and improve the disability.
Cervical
Cervical Spine Anatomy
The spine, also called the back bone, plays a vital role in stability, smooth movement and protection of the delicate spinal cord. It is made up of bony segments called vertebra with fibrous tissue called intervertebral discs between them. The vertebra and discs form the spinal column from the head to the pelvis, giving symmetry and support to the body.
A single vertebra is made up of two parts, the front portion is called the body and the back portion is referred to as the vertebral or neural arch. The body is cylindrical in shape, strong and stable. Two strong pedicle bones join the vertebral arch to the body of the vertebrae.
The laminae of the vertebra can be described as a pair of flat arched bones that form a component of the vertebral arch. The transverse processes spread out from the side of the pedicles, like wings, and help to anchor the surrounding muscle to the vertebral arch. The spinous process forms a steeple at the apex of the laminae, and is the part of our spine that is felt directly under the skin.
Spinal canal is formed by the placement of single vertebral foramina one on top of the other to form a canal. The purpose of the canal is to create a bony casing from the head to the lower back through which the spinal cord passes.
The spine can be divided into 4 parts: cervical, thoracic, lumber and sacral region. The cervical spine comprises the first 7 vertebrae of the spinal column, which form the neck.
The cervical spine is highly mobile compared to other regions of the spine such as thoracic or lumbar spine. In contrast to other parts of the spine, the cervical spine has transverse foramina in each vertebra through which the vertebral arteries supply blood to the brain.
Based on the structural diversity in the cervical spine, it can be divided into two parts: upper and lower cervical spine.
Upper cervical spine
The upper cervical spine comprises of the atlas (C1) and axis (C2), which are different from rest of the cervical vertebrae. The atlas vertebra articulates with the occiput superiorly at the atlanto-occipital joint and with the axis inferiorly at the atlantoaxial joint. Generally, the atlantoaxial joint is accountable for half of the cervical rotational movements; while the atlanto-occipital joint is responsible for half of the flexion and extension movements of the neck.
Atlas (C1)
In contrast to other vertebrae, the atlas is ring-shaped without a body. The odontoid process, or dens of the axis, represents the fused remnants of the body of the atlas. The transverse ligament firmly opposes the odontoid process to the posterior portion of the anterior arch of atlas and provides stability to the atlantoaxial joint.
The atlas comprises of a thick anterior arch, a thin posterior arch, two prominent lateral masses, and two transverse processes. The transverse process surrounds the transverse foramen, through which the vertebral artery passes. A zygapophyseal joint is present on the superior and inferior aspect of the lateral mass. The superior articular facets articulate with the occipital condyles and are kidney-shaped, concave, projecting upward and inward, while the inferior articular facets are comparatively flat projecting downward and inward and articulate with the superior facets of the axis.
Axis (C2)
The axis possesses a large vertebral body with the odontoid process or dens. The axis also has heavy pedicles, laminae, and transverse processes, which help in the attachment of muscles.
Lower cervical spine
The remaining five cervical vertebrae, C3-C7, form the lower cervical spine. They are similar to each other but distinct from C1 and C2. Each of these cervical vertebrae has a body with a concave superior surface and convex inferior surface. The superior surfaces of the bodies have raised processes called uncinate processes that articulate with the inferior lateral portion of the vertebral body present above, called echancrure or anvil.
The C3-C6 vertebrae have bifid spinous processes, meaning they are split in two parts, whereas C7 has a nonbifid, rounded spinous process.
Intervertebral Disc
The intervertebral discs are flat and round, present between the lumbar vertebrae and act as shock absorbers when you walk or run. There is a soft, gelatinous material in the center (nucleus pulposus) which is encased in strong elastic tissue forming a ring around it called annulus fibrosus.
Facet Joint
Facet joints are synovial joints which give the spine it’s flexibility by sliding on the articular processes of the vertebra below. The joint capsules are quite loose in the cervical region, compared to other parts of the spine, to facilitate smooth movement.